Postpartum is forever. However, the things you do in the first 8 weeks can lay the foundation for how you’ll feel in the months and years that follow. The challenge? The physical and emotional demands of your new motherhood.
To make things easier (and to not just add another task to your plate), here’s a simple, actionable guide to help you prioritize healing — without the overwhelm – with postpartum pelvic floor exercises for the first 8 weeks.
Understanding postpartum recovery
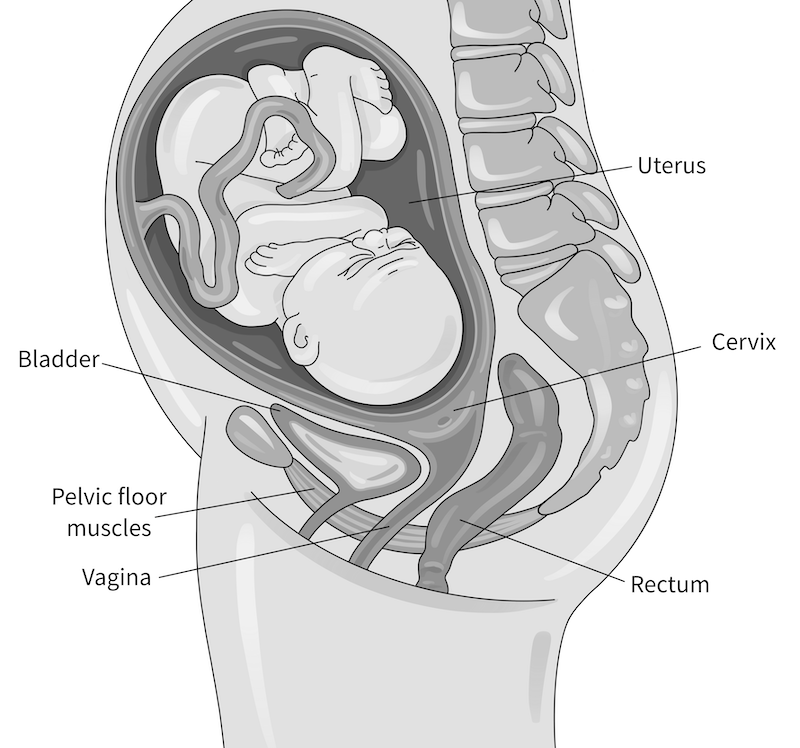
Your body has been through a lot of changes during pregnancy and childbirth, and your pelvic muscles — the hammock of muscles that support your pelvic organs (bladder, uterus, and bowels) — have taken on a huge load.
During pregnancy, these muscles stretch and adapt to support a growing baby. During vaginal birth, they endure even more stress and strain. In fact, 9 in 10 women1 experience perineal tearing with vaginal delivery. Even cesarean births involve core and pelvic floor strain. Unfortunately, these injuries can lead to different pelvic floor disorders3, including bowel leakage, urinary leakage, and pelvic organ prolapse.
If this sounds overwhelming, know this: there’s no way to guarantee you’ll avoid injury during birth. The key is taking the time to heal well during your post-birth recovery. Here’s how to start.
Weeks 0 to 2: Gentle activation and healing
The first 2 weeks after birth are all about healing, supporting your bladder and bowel function, and gently reactivating your pelvic floor and deep core muscles. Some mindful movement can make a big difference.
Gentle postpartum pelvic floor exercises
Since your pelvic floor naturally engages during breathing, a simple way to reconnect is through diaphragmatic breathing. This will improve circulation, reduce swelling, and reestablish muscle strength and coordination:
- Sit with your feet flat on the floor.
- Take a deep breath in, allowing your ribcage to expand and your pelvic floor to relax.
- Exhale and gently draw your pelvic floor muscles inward — like a subtle Kegel, imagining sipping up a thick smoothie with your vagina.
- Repeat for 10 breaths.
Safe early movements
Keep movement light and gentle:
- Postural support: Sit with good posture, especially while feeding your baby, to protect your back and pelvic area. Try sitting upright with your feet on the floor and pillows supporting your back. You can also use pillows to bring your baby up to your nipple, instead of bending down to reach them.
- Optimal body mechanics: When lifting your baby, engage your deep abs and pelvic floor to protect your back and exhale as you lift.
- Short walks: This type of physical activity can boost circulation, prevent blood clots, and encourage core engagement.
Healing and self-care
To ease vulvar swelling and pain:
- Use a peri bottle for gentle cleansing after using the bathroom for pees and poops.
- Apply cold packs or a “padsicle” to the vulvar area for pain relief.
- Wear supportive, slightly compressive undergarments. My fave is the Lovesteady Bloomers.
- Take sitz baths to soothe soreness.
Bladder and bowel health
Some urinary incontinence, leakage or discomfort is normal after birth, but symptoms should improve each day. Support your recovery with:
- Hydration: Drink more water than you think you need—it’s essential for lactation, bowel function, and healing.
- A squatty potty: This helps with easier bowel movements and emptying your bladder more comfortably.
- Fiber-rich foods: Whole food sources of fiber are best, but supplements can help too.
Weeks 2 to 4: Restoring function and strength
By 2 weeks postpartum, your body is adjusting, but healing is still in progress. This phase focuses on supporting your vulvar and pelvic floor health and gradually increasing activity.
Progressive postpartum pelvic floor exercises
You may notice improvements in bladder and bowel function, but lingering leakage or urgency could point to pelvic floor dysfunction. If symptoms persist, a pelvic floor physical therapist (PT) can help. For now, try these postpartum pelvic floor exercises:
- Seated Kegels: Engage and fully release your pelvic floor muscles in a pain-free way.
- Sit-to-stand with Kegel: Lightly activate your pelvic floor and deep core as you stand up.
- Belly lifts (on hands and knees): Support gentle core activation.
- Walking progression: Gradually increase distance and speed as long as you’re pain-free — your pelvic floor exercises as you walk
Pay attention to your body. If you experience pain, pressure, increased leakage, or bleeding during or after exercise, scale back and check in with your OB or pelvic floor PT before progressing further.
Caring for your vulva
Pregnancy and postpartum hormones — especially with breastfeeding — can lead to vaginal dryness. Applying vitamin E oil to your vulvar tissues may help, and your OB can discuss options like topical estrogen if needed.
Nutrition and hydration
Fuel your recovery with:
- Healthy fats, lean proteins, and complex carbs to support healing and energy levels.
- Plenty of fluids, especially if you’re breastfeeding.
Weeks 4 to 8: Strength, scar care, and returning to activity
By 4 to 8 weeks postpartum, healing is steady, and you may feel ready for more exercise. This phase focuses on scar care, sexual health, and reintroducing exercise safely.
Scar care and returning to sex
If you had a perineal tear or C-section, gentle scar massage (once fully healed) can help reduce tightness, improve mobility, and lower the risk of pain, adhesions, and other long-term issues.4
Around this time, you may get clearance for sex. (Deep breath!) Because of things like changing hormones and healing and sensitive vaginal tissues, sex can be painful. If you’re ready, try:
- Proactively using lubricant during vaginal intercourse
- Perineal scar massage to ease discomfort from scar tissue
- Allowing plenty of foreplay to enhance arousal and lubrication
- Addressing pelvic floor tension or scar pain if pain during sex persists
Advancing postpartum pelvic floor exercises
With medical clearance, start low-impact postpartum pelvic floor exercises like:
- Walking, gentle core work, and pelvic floor muscle strengthening.
- Avoiding high-impact activities (running, HIIT, heavy lifting) until at least 12 weeks postpartum.
Again, pay attention to symptoms — if you notice pain, leakage, or increased bleeding, scale back and contact your medical provider.
Pelvic floor therapy postpartum
Your postpartum journey is unique, and healing isn’t a race. By focusing on rest, movement, and self-care, you’re setting yourself up for a strong recovery.
If symptoms like pelvic pain, leakage, or discomfort persist, postpartum pelvic floor therapy can be a great option. You can see a pelvic floor physical therapist as soon as the first few days postpartum. They’ll help guide you through your recovery with a treatment plan that’s designed specifically for you, your pregnancy and postpartum history, and goals during your recovery.
Another great option? Check out the Childbirth Recovery Program in the V-Hive, where you’ll find expert-led postpartum pelvic floor exercises. You can start today with a free trial membership and get instant access to every workout.
References
- Okeahialam N.A., et al. (2024). The prevention of perineal trauma during vaginal birth. Am J Obstet Gynecol.
- Pessoa P., et al. (2024). Prevalence of levator ani muscle injuries in primiparous women after delivery and their influence on pelvic floor disorders-systematic review. Neurourol Urodyn.
- Barca J.A., et al. (2021). Pelvic floor morbidity following vaginal delivery versus cesarean delivery: Systematic review and meta-analysis. J Clin Med.
- Alpay Z., et al. (2008). Postoperative adhesions: from formation to prevention. Semin Reprod Med.